GMP: ANSM publishes the French translation of Annex 1. How can you adapt your action plans?
On 15 July, ANSM notified the publication online of the French translation of Annex 1 of the Good Manufacturing Practices (GMP) for medicinal products for human use.
The European Commission had initially re-examined this chapter, dedicated to the specificities of the production of aseptic medicinal products, in order to standardise manufacturing practices on an international scale. Since its publication on EudraLex in August 2022, manufacturers have been complying with this original version, which has been in force since August 2023.
The transposition of the revised Annex 1 of the European Good Manufacturing Process (GMP) is intended to remove any ambiguities about the enforceability of the text, since it effectively brings it into line with French law. For French manufacturers, this translated version should also clarify ambiguous wording and points in the original text.
What impact will the revision of Annex 1 have on companies? How can it be implemented on production sites? What are the challenges of GMP compliance? Lugan Consulting has the answers.
GMP: revision of Annex 1 on the manufacture of sterile medicinal products
Appendix 1 lists the fundamental principles for the manufacture of sterile medicinal products. It was originally published in 1971 with the aim of providing an exhaustive manufacturing guide. It has already undergone several revisions.
The most recent revision, in 2022, was initiated to take account of the impact of the Covid crisis, regulatory changes and the increasing use of new technologies for the manufacture of sterile medicinal products.
A further update was needed to incorporate manufacturing strategies based on new technologies, to specify sterilisation methods and to take account of rapid analysis techniques.
The new edition therefore includes 11 new sections, as well as a glossary for greater clarity.
Scope of GMP Annex 1
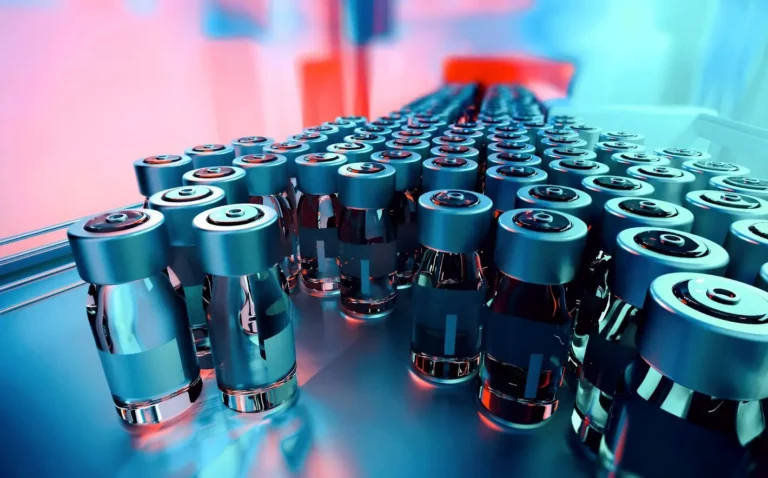
‘Sterile’ refers to medicines that are “uncontaminated by micro-organisms” (microbes, particles, bacteria, fungi, viruses, etc.). The absence of these elements is essential to guarantee the safety and efficacy of aseptic preparations, as their contamination could lead to serious or even fatal infections in patients.
When we talk about the manufacture of sterile products, we are talking about products, different presentations, processes and technologies. These include
- Terminal sterilised medicinal products (ampoules and vials for injection, intravenous solutions, sterile eye drops and ointments, etc.)
- Medicinal products prepared in controlled atmosphere areas (vaccines, blood-derived medicinal products, medicinal products administered by intravenous or intrathecal injection, ophthalmic medicinal products, sterile topical medicinal products, etc.).
Changes brought about by the update of GMP Annex 1
The introduction of the new Annex 1 has led to some major changes. The directives focus on preventing contamination, without minimising the detection or removal stages. The changes relate to 4 areas:
Taking technology into account
One of the recommendations (section 2.1) highlights the appropriate use of technology in aseptic production operations: restricted access barrier systems (RABS), isolators, single-use technologies, robotic systems, rapid or alternative methods, continuous monitoring systems, etc., in order to be able to rapidly detect any contamination of the environment or the product during the manufacturing process. For manufacturers, the introduction of technology can also be a solution to improve the reliability of operations or save time, such as the automation of candling, for example.
However, the introduction of technology is the first step towards the future of aseptic manufacturing, with human presence reduced to a minimum (use of isotechnology). It is clear that the risks of contamination inherent in the latter can be reduced by introducing robotics, or even Artificial Intelligence. The big names, such as Sanofi, have already done this.
However, the emphasis is on the fact that these technologies and automated monitoring systems need to be operated by staff who are trained and qualified to use them.
In all cases, the use of the technologies must be documented in the CCS, another new feature of the update.
Contamination Control Strategy (CCS)
This is one of the major changes to be taken into account in this new version. CCS is a systematic, documented approach implemented as part of a policy to ensure and prevent the risks of contamination in the manufacture of sterile medicinal products. In practice, establishing this strategy involves drawing up technical and organisational documentation defining the means of control. It is then used as a reference for risk assessment.
The key elements of an effective CCS are :
- Risk assessment: Identify potential sources of contamination in all aspects of manufacturing, including raw materials, equipment, personnel and production environments.
- Control measures: implement appropriate protocols to eliminate or minimise identified risks, such as disinfection, sterilisation and environmental monitoring.
- Monitoring: regularly observing the effectiveness of control measures and the presence of contaminants in environments and products.
- Review and update: regularly review and update the CCS to take account of changes in manufacturing processes, risks and scientific knowledge.
The update recommends the implementation of a SCC, while stressing that manufacturers of sterile medicinal products must adapt it to their specific facilities and products. The SCC must be documented and applied by qualified personnel. They must have sufficient knowledge of sterilisation and microbiology at all levels of the organisation.
Compliance with the CCS is now one of the inspection points monitored by the regulatory authorities.
Quality Risk Management (QRM)
Update 2024 does not introduce any new QRM requirements, but aims to achieve international harmonisation of processes, operations and limits. It therefore covers a wide range of subjects: the layout of cleanrooms, equipment and manufacturing methods, staff training, choice of clothing, cleaning and disinfection procedures, qualifications and monitoring systems, etc.
Evidence of the implementation of risk management is characterised by :
- Appropriate design of plant, equipment and manufacturing processes.
- The creation of procedures adapted to the manufacturing activity specific to the type of product being manufactured.
- Setting up a monitoring system.
QRM becomes a systematic and proactive approach, to be carried out throughout the sterile medicinal product manufacturing process (this is a link between the manufacture of sterile medicinal products and the ICH Q9 guide).
Pharmaceutical Quality System (PQS)
The major revision of 2022 introduced a new approach to the Pharmaceutical Quality System for the manufacture of these products. This development is based on the ICH Q10 guidelines and focuses on the following points:
- Risk-based approach: manufacturers must introduce a thorough assessment of the risks of microbial, particulate and endotoxin/pyrogen contamination throughout the manufacturing process. The implementation of continuous monitoring and control measures is recommended.
- Responsibility and expertise: the facility’s management must make a clear commitment to the PQS. It must ensure that the PQS is implemented and maintained effectively, particularly through staff training (microbiology, use of machines, operating protocols, cleaning, etc.) to ensure the quality of sterile products.
- Documentation and records: the SQP is based on the design of a comprehensive documentation system. This includes risk assessment, control measures, monitoring, training, etc., as well as the recording of activities and decisions relating to the PQS. This enables events to be reconstructed and compliance to be demonstrated.
- Change management: setting up a rigorous process for assessing, approving and implementing changes to the PQS, ensuring that risks are kept under control.
- Inspection and audit: manufacturers must carry out regular self-inspection, as well as external quality audits led by independent experts to confirm compliance with the PQS and regulatory requirements. In the event of non-compliance with procedures, an investigation must be carried out before the batch is released, to justify the reasons for including or excluding it.

Impact of the update
Changes in quality and control processes will have an impact on various points in the production chain:
- Induced changes to organisation, operations or equipment may slow down production line speeds while they are implemented and validated.
- Clinical trials and marketing authorisations could potentially be suspended.
- The updating of Annex 1 is a strong incentive to implement risk management coupled with environmental monitoring, which requires test cycles and extensive documentation to be drawn up.
In this context, the design of manufacturing and production processes and their validation will automatically take longer to develop.
It is important to stress that these impacts and their scope may vary depending on the specific features of the products manufactured, but also on each manufacturer’s ability to adapt quickly. In all cases, it is necessary to assess upstream the repercussions of the new Annex 1 requirements on processes and lead times.
Point 8.123: freeze-dryers
Implementation of this point is scheduled for 25 August 2024. The unusual delay of two years has been granted to manufacturers to give them time to adapt technically to the new requirements.
As far as freeze-dryers are concerned, the trend is towards fully automated loading. Here again, the aim is to avoid human interaction in the sequence from pre-capping the bottle to entry into the freeze-dryer. This precise point needs to be considered in detail for sites with systems that are not compatible with the level of flexibility in production.
One of the points in question here is automatic tray loading. The new directives do not require this system to be discontinued, but this decision has a cost in terms of the disinfection processes required. The daily cost of sterilising around a hundred trays probably exceeds, in the long term, the cost of loading trays directly onto plates. We therefore need to think strategically at all levels: is it essential to make an investment? Change premises?
The English version had already been greatly simplified. The French translation provides French-speaking customers with a coherent reference system that is in line with the jurisdictions to which they are answerable.
GMP issues in 2024
For manufacturers of sterile medicinal products, compliance with GMP and, more specifically, Annex 1, raises a number of issues.
First and foremost, of course, is patient safety. That’s the crux of the matter.
Then there is the question of brand image. Being compliant means being at the cutting edge and demonstrating flexibility: a strong argument for winning the trust of customers and enjoying a viable image.
In addition, the PIC/S harmonises inspection practices and updates the reference framework for those in charge of compliance audits: following the directives as quickly as possible means avoiding the impact of non-compliance.
Lastly, ANSM reports highlight a clear increase in GMP non-compliance as a factor contributing to shortages:
Since 2019, declarations of stock-outs and risks of stock-outs have exploded (3370 declarations recorded in 2023. There were fewer than 500 in 2014). Non-compliance with GMP represents a cause that has tripled since last year (from 20 to 64). Meeting GMP requirements means avoiding disruption to production and remaining competitive.
Measures to be taken to comply with the new requirements
Faced with changing procedures, professionals in the sector must, if they have not already done so, implement measures in a methodical and considered manner:
👉First, understand all the changes contained in Appendix 1 by studying it closely.
👉 Identify the existing gaps between the expectations and the reality of the production site and draw up a list, point by point, of the actual non-conformities.
👉 From this list, identify the cases for which an immediate or short-term solution can be envisaged. These are often inexpensive measures.
👉 Plan the action needed to make improvements. Document developments.
👉 Train teams: to ensure that operational staff work within the constraints required by the new directives, they need to be clearly informed of the points of change.
👉Encourage the use of new technologies on the production line and train staff in their use. Plug and play’ technologies can be considered for greater ease of use.
👉 Don’t neglect elements external to the production line: carry out an audit of suppliers, raw materials and transport. The sterility of products must be ensured until they are received.
👉As part of the principle of continuous improvement, carry out periodic and random audits to ensure the conformity of your production. If an anomaly is detected, report it, record it, investigate its origin and take the necessary measures as quickly as possible.
How can you ensure that GMPs are properly implemented?
If you are one of the companies that preferred to wait for the French publication of Annex 1 before embarking on a compliance strategy, it is clear that time is running out to be 100% compliant by the autumn. Complying with GMP requires a certain amount of inertia, but if a company is audited, it must be able to demonstrate that it has taken the necessary steps. So it’s not too late!
Choose to move in the direction of Annex 1 by taking as many actions as possible as quickly as possible. Have at least a partial roadmap. Be careful not to hide behind a lack of skills or functions to justify why nothing has been put in place. Eventually, this argument will no longer be tolerated by the supervisory authorities.
If you don’t have qualified staff, you can turn to the services of specialist external consultants, such as those offered by LUGAN CONSULTING, to get you started on the road to compliance. Don’t risk an ANSM injunction!
Aren’t you a manufacturer of sterile products? The update to Annex 1 applies to you too! The text emphasises that the principles set out in the standard should be taken into consideration for all types of pharmaceutical production. The requirements of sterile production are such that the instructions in appendix 1 can only be of benefit to all sectors of pharmaceutical production.
Our expertise in pharmaceutical production quality meets the needs of all those involved in production.